Evidence Shows Philadelphia’s Indoor Vaccine Mandate Didn’t Work
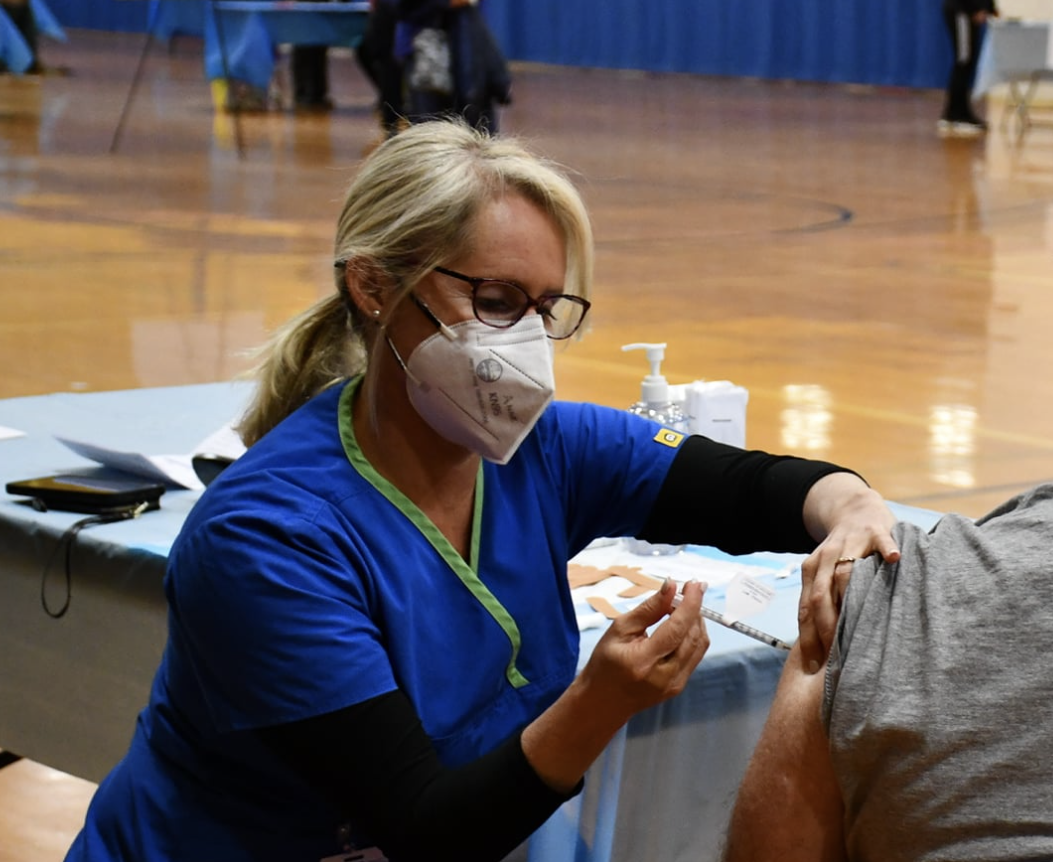
When Saba Tedla, the owner of several popular Philadelphia eateries, let some of her longtime kitchen staff go last year, she didn’t have any choice. Under the city’s vaccine mandate, employees who declined the COVID-19 shot were barred from working indoors at a restaurant. Similar stories can be found across the city. Facing a unique threat to public health, government officials believed the policy would make the city safer.
With the benefit of hindsight and data, we now know otherwise. A new study conducted by one author of this op-ed found no evidence that Philadelphia’s vaccine mandate led more people to get vaccinated or lessened the pandemic’s impact.
At the time, city officials insisted indoor vaccine mandates would save lives. “This winter looks like it could be very difficult,” said Philadelphia Health Commissioner Cheryl Bettigole in December 2021, when the mandate was announced. “We have to do something to slow the spread now before it’s too late.” Health experts were right to be worried. The Omicron wave was tearing through the U.S., killing many Philadelphians.
Sadly, good intentions are not enough to produce positive outcomes.
The analysis compared the effects of vaccine mandates in nine major U.S. cities, including Philadelphia, with data taken during the pandemic in hundreds of other cities. Whether it was vaccination rates, COVID-19 cases, or COVID-19 deaths, we found no statistically detectable effect of the vaccine mandate.
To be clear, the research doesn’t suggest that COVID-19 vaccination is ineffective or unsafe – merely that vaccination mandates did not meet their goals.
The results surprised us, especially since vaccine mandates in Canadian provinces and some European countries have been linked to increased vaccination rates. Why weren’t similar policies effective here? We can think of a few possibilities.
The first is simply common sense. Unvaccinated individuals could enjoy indoor activities simply by traveling beyond the city limits. That is consistent with findings that in larger geographic jurisdictions, compliance with such mandates tended to be higher.
Second, vaccine mandates, paradoxically, may have exacerbated opposition to getting the shot. As recent research has pointed out, “insights from behavioral psychology suggest that these policies are likely to entrench distrust and provoke reactance – a motivation to counter an unreasonable threat to one’s freedom.”
Whether vaccine mandates were unreasonable threats to freedom is, of course, debatable. But it is an inescapable fact that much of the population regarded the mandates as impinging on their rights. In the end, for every Philadelphian who was coaxed into getting vaccinated by the mandate, we estimate that someone else was deterred from doing so.
Third, vaccination mandates may have triggered the “Peltzman effect,” the tendency to make riskier decisions when safety measures are implemented. In this case, the mandates may have fostered a harmful sense of complacency among vaccinated patrons of indoor venues. Thinking that requiring vaccinations eliminated infection risk, some people may have let their guard down in other ways – by visiting more crowded spaces, perhaps, or taking fewer precautions to mask and socially distance.
Our findings add to a long list of COVID-19 policy blunders and missteps – from depriving nursing home residents of relatively safe contact with loved ones to enforcing lengthy school closures in low-risk areas. Public officials were in a difficult position, but too often, they enacted draconian measures based on weak evidence.
Indoor vaccine mandates were among the most restrictive policies ever adopted in the United States. It was easy–perhaps too easy– to believe that the benefits outweighed the costs. But in this case, they didn’t.
Please follow DVJournal on social media: Twitter@DVJournal or Facebook.com/DelawareValleyJournal